The future is
mobile
Photos
Stephan Minx

When surgeon Dr. Sven Seifert enters the OR, he exudes confidence and poise. That’s not surprising, considering the number of operations he has successfully performed in the past decades. Seifert has headed the Clinic of Thoracic, Vascular and Endovascular Surgery at the municipal hospital in Chemnitz, Germany, for seven years and has over twenty years of surgical experience.

While Seifert’s demeanor communicates “commander-in-chief”, he’s still approachable. The surgeon started working with Ziehm Imaging mobile C‑arms in 1996 and has stayed loyal to the manufacturer ever since. Today, three procedures are slated here in Chemnitz, all of which will take place in hybrid operating rooms. Seifert and his team’s first procedure of the day will be an endovascular abdominal aortic aneurysm repair (EVAR). The operation is one of the standard procedures performed in the two vascular surgery hybrid operating rooms in Chemnitz.
Seifert performed his first surgical procedure in a hybrid OR in 2007 and is considered to be one of the pioneers of the “hybrid movement”. Hybrid surgery was designed to combine the conventional surgical setting with medical imaging in the same room. This combination reduces risks and stress for the patient and also streamlines the surgical workflow. Hybrid operations are now the standard procedure for complex procedures with high intraoperative imaging requirements. They are most commonly used for cardiac and vascular surgery, as well as for neurosurgery. Procedures involving the aorta are risky, time-consuming and radiation-intensive. The hybrid OR offers enormous advantages for this type of surgery, Seifert explains. The hybrid OR is the only setting that ensures the combination of hygiene class 1A and imaging, which is otherwise found only in radiological units. The biggest advantage of the special OR is that the patient needs to undergo only one surgical procedure, Seifert says.
The mobile hybrid OR
“Since 2014, we have had a hybrid OR with a fixed angiography unit here in Chemnitz. The hybrid OR with a mobile C‑arm is directly adjacent,” Seifert adds. For a long time, the intraoperative image quality of the mobile C‑arm was considered to be inadequate for hybrid applications in vascular surgery, where it is crucial to precisely visualize even the tiniest anatomical structures. This has changed in recent years, Seifert says. “The image quality of mobile C‑arms is now outstanding.”
Seifert especially appreciates the fact “that with a mobile C‑arm, we are able to completely change the surgical set-up during the procedure and also change sides if need be.” In addition, the mobile C‑arm can also be used in another room as needed. Seifert explains that this has made imaging more efficient and in turn, more cost-effective. In addition to flexible room scheduling, the surgeon sees the substantially lower investment costs as a particular advantage. Setting up and equipping a standard hybrid operating room takes time and requires considerable construction efforts. In contrast, the mobile C‑arm’s lower installation and operating costs open up possibilities for smaller hospitals or those on tight budgets to perform hybrid procedures as well, Seifert says. In terms of technology, the mobile C‑arm also offers a number of advantages for vascular surgery, Seifert explains. “For me, the effortless way the collimators work and the rotation of the clinical image in the operation setting are both real advantages.”

Seifert’s mobile hybrid OR features a Ziehm Vision RFD Hybrid Edition1, a mobile C‑arm that has been specifically tailored for use in a hybrid OR. “The C‑arm has a very special shape and our pet name for it is ‘The Turtle’.” Seifert is referring to the modern design of the flat-panel detector, whose semi-circular shape in fact does resemble a turtle, to some extent. The Ziehm Vision RFD Hybrid Edition combines a number of highlights that Seifert considers to be particularly important for a mobile C‑arm, especially its full motorization in four axes that can be controlled directly from the sterile field via two joysticks. “This feature makes using it effortless for surgeons and their teams.”
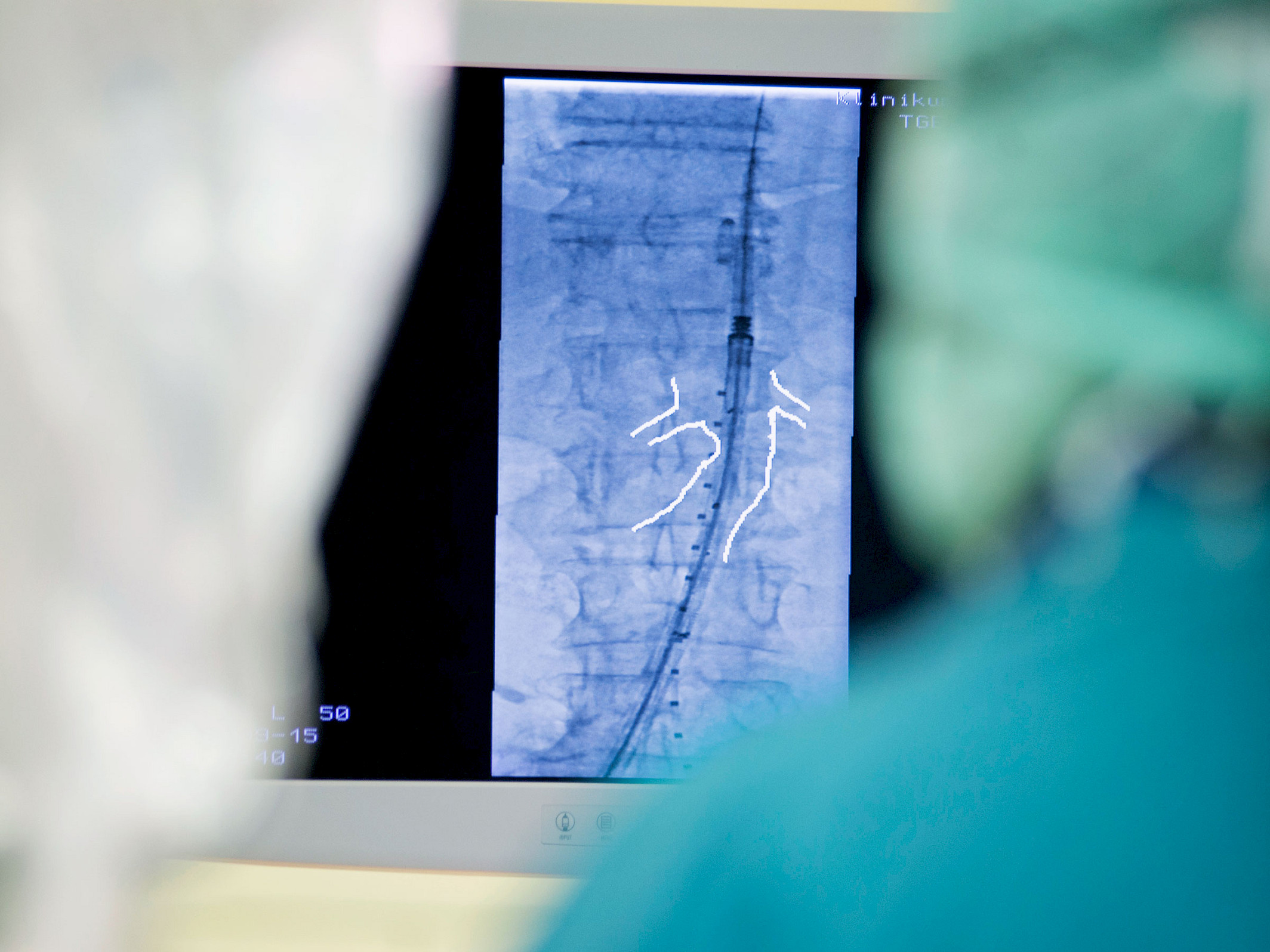
During the procedure, Seifert uses the wireless footswitch to pinpoint the position at the patient that is best suited for his work. When he changes his operating position, he simply takes the footswitch with him. Safety and efficiency are particularly important in an operating room, Seifert says. That’s why he likes to use the Anatomical Marking Tool when he performs EVAR. The “ingenious drawing tool”, as Seifert describes it, allows him to precisely trace the course of the internal iliac artery in the live display of the digital subtraction angiography (DSA). Seifert simply uses his forceps as a stylus to input the necessary information onto the clinical image of the C‑arm on the sterilely wrapped touchpad. In so doing, Seifert marks a sort of “canal” that can be viewed live on all his monitors and which shows him precisely where the aortic stent must be released in the superimposed fluoroscopy. “This makes us more certain that we have positioned the prosthesis properly and it offers the advantage of considerably less radiation,” Seifert adds.

During EVAR, Seifert applies CO2 to visualize the contrast. Pressure is used to guide the CO2 into the artery, where it forms a gas bubble and pushes the blood flow of the vessels ahead of it. Contrary to conventional contrast media containing iodine, CO2 does not pose the risk of an allergic reaction. Seifert was one of the first surgeons to incorporate CO2 in clinical routine due to its better tolerability: “CO2 can be used as a contrast agent in any patient. It does not burden the thyroid and is not expelled through the kidneys.” Seifert plans to eliminate the use of conventional contrast media in as many surgical procedures as possible to reduce the risk to the patients. The increase in common conditions such as obesity and diabetes has boosted the demand for CO2 angiography. For many patients with these conditions, iodinated contrast media are not an option.
In Seifert’s view, the Ziehm Vision RFD Hybrid Edition offers the ideal imaging system for CO2 angiography. “We are working with one of the few systems that performs immediate inversion of the subtraction image, which allows us to ideally visualize the contrast.” The rapid inversion of the negative contrast – in other words, the possibility to make the CO2 within the vessels appear black – enables the angiography images to be displayed in the manner in which the surgeon is accustomed. As he looks at the final image of the surgery, Seifert is pleased with the high quality of CO2 angiography with the Ziehm Vision RFD Hybrid Edition. “We have succeeded in placing the stent graft in an ideal position, without using conventional contrast media.”

Seifert is satisfied as he wraps up the procedure. Despite the heavily calcified arteries and the difficult morphology of the surgical site, the procedure has been successful. The patient has been spared a postoperative follow-up scan and a possible additional operation. As Seifert puts it, his “Turtle” has done an outstanding job. “The future belongs to the mobile hybrid OR. The mobile C‑arm with the image quality we have experienced today offers a space-saving and cost-efficient alternative to a fixed installed unit.”
Disclaimer
1
Ziehm Vision RFD Hybrid Edition represents a group of optional hardware and software that creates an option package on the device named Ziehm Vision RFD.
More information on Ziehm Vision RFD Hybrid Edition
—
This clinical story was published in issue 1 (2017).
Download issue 1 as PDF